
Academics
Our DO program prepares you for a practice that values the ongoing health of your patients as much as curing disease.
Our comprehensive curriculum integrates basic science and clinical medicine concepts with an osteopathic focus using an inter-professional, community-centered model.
Our Education Digs Deep
TUC's Doctor of Osteopathic Medicine education is built upon a curriculum that integrates the best tenets of osteopathic medicine. We focus on primary care, but we are not defined by it, and TUC's DO graduates divide almost equally between careers in primary care and specialty medicine. You’ll find a focus on structural competency throughout our curriculum. It's one of our core competencies and we’re the only medical school that has structural competency as one of our program learning outcomes. It’s that important to us.
So What is Structural Competency?
Structural competency relates to the social and economic factors that impact your patients’ health, beyond genetics. For example, when you learn about pediatric diabetes you’ll learn the epidemiology of the disease and in which individuals type 2 diabetes is more common – ethnicities such as Native American, Hispanic, and African American – as you would in any medical school. But then we encourage you to ask “Why? Why is it more common in these groups?” We want you to learn about their housing situations and healthcare deserts and food assistance programs, and understand the social determinants of health that often have a greater impact on health than genetics, and sets up these groups to have a higher rate of diabetes.
Armed with that knowledge and understanding, as a physician you are also in a better position to help your patients and advocate for them. That can mean advocating for policy change or community gardens or the awareness of the challenges they face and what might be accessible and realistic for your patient in addressing their issue.
You can be sure you will leave TUC's DO program with attributes found in only the best physicians, with the ability to see each patient as the unique individual that they are, with their own unique circumstances. You will be prepared to pursue your choice of careers in medicine and really help your patients.
Our Education Thinks Big
Our DO program offers innovative education, active community involvement and a focus on public health and translational research. And we're not the only ones that think our curriculum is innovative! Our Curricular Innovation Awards include:
- In 2021, Mr. Glenn Davis received the AACOM Innovation in the Development of Enduring Educational Materials Award for SCOR – An Innovative Osteopathic Core Competency Assessment System
- Also in 2018, Dr. Tami Hendriksz received the AACOM Innovation in the Development of Enduring Educational Materials Award for her design of the Patient Perspectives curriculum.
- In 2017 Dr. Jennifer Weiss received the American Association of Colleges of Osteopathic Medicine (AACOM) Marguerite Ellison Prize for Innovations in Clinical Education for her design of the Year 3 Clinical Distinction program. In 2018 she and her colleagues were awarded the Stephen Abrahamson Award for Outstanding Innovations at the Innovations in Medical Education Conference.
- In 2016 Dr. Stacey Pierce-Talsma & Joel Talsma received the American Association of Colleges of Osteopathic Medicine (AACOM) Innovation in Osteopathic Medical Distinctiveness Award for their COAR: Clinical Skills, Osteopathic Manipulative Medicine, Anatomy, Radiology curriculum
DO students engage in a hands-on approach from day one and learn to tackle some of the biggest health issues in our nation from an individual patient perspective to community health and global health.
Part of what makes our curriculum so unique is our focus on structural competency. You will learn about healthcare inequities and disparities, as well as some of the reasons why they exist, and what you can do to best help your future patients.
Our Curriculum
Preclinical Education
In your first two years, you’ll blend classroom learning and early clinical experiences to prepare to work in clinical settings. Each semester you’ll take courses along three tracks: integrated sciences, osteopathic doctoring and osteopathic manipulative medicine. Along with an emphasis on structural competency, our curriculum also covers the American Osteopathic Association (AOA) core competencies:
- Osteopathic Principles and Practices
- Medical Knowledge
- Patient Care
- Interpersonal and Communication Skills
- Professionalism
- Practice-Based Learning and Improvement
- Systems-Based Practice
Our simulated patient care lab allows student-doctors to practice what they've learned while facing a series of real-world scenarios. The patient is an actor, portraying a real-world patient scenario so the reactions of patient and physician are as real as can be.
Integrated science courses are organized into body systems so, for example, you will learn everything that you need to know about the cardiovascular system in an integrated manner before moving on to the respiratory system.
Osteopathic doctoring courses provide a strong foundation in professionalism, medical practice, clinical skills, ethics, humanities and early clinical experience. You’ll learn to apply basic science and clinical knowledge. You’ll interact with real and simulated patients, patients in community and clinical settings.
Osteopathic manipulative medicine courses allow you to develop osteopathic thinking, by integrating osteopathic manipulative treatment into the diagnosis and treatment of patients.
Preclinical Courses: First Year
Fundamentals of Osteopathic Medicine (13 units)
The Fundamentals of Osteopathic Medicine course presents the scientific basis of clinical medicine. Students will learn the aspects of biochemistry, anatomy, physiology, histology, embryology, genetics, pharmacology, pathology, microbiology and immunology that are necessary to begin study of the organ and tissue systems of the body.
Osteopathic Doctoring 1 (3.5 units)
The Osteopathic Doctoring course is an integrated and comprehensive course that will span the first two years of osteopathic medical school curriculum. It provides the basic cognitive and kinesthetic skills for future physicians to provide medical attention in a competent and professionally compassionate fashion. This course provides the foundation for students to practice the art and expanding science of osteopathic medicine through focusing on clinical skills (such as, patient interviewing and physical examination), clinical reasoning (the process by which physicians’ are able to choose the most appropriate individualized diagnosis and treatment plan), professional practice (the development of behaviors and practices that embody the expectations of an osteopathic medical professional), and clinical integration (the ability to apply basic science knowledge in all aspects of clinical practice). This course utilizes standardized and real patients to help increase early clinical exposure and allows for solidification of the application of basic sciences in clinical practice.
Osteopathic Principles and Practices 1 (3.5 units)
The Osteopathic Principles and Practices 1 course is the first of a four semester cumulative body of basic knowledge and skills that spans the first two years of your Osteopathic medical school curriculum. It is designed to reinforce the basic tenets, philosophy, principles, and practice of osteopathic medicine. Though the course does contain all the inclusive knowledge to be successful in the National Board of Osteopathic Medical Examiners board exams, it is primarily designed to provide the foundation (as well as more advanced theoretical and psychomotor skills) for future osteopathic physicians to integrate osteopathic philosophy, diagnosis, and treatment in a competent compassionate and professional manner into patient care.
Integrated Systems: The Cardiovascular, Respiratory and Renal Systems (14.5 units)
The Integrated Systems Cardiovascular-Respiratory-Renal course (IS-CVRR) develops a deep understanding of the biological, diagnostic and therapeutic principles that produce optimal health and allow well-informed patient care. In addition, a knowledge base in clinical and basic science will optimize success on board examinations and clinical rotations. Specifically, the course presents physiology, anatomy, pathology, pharmacology, microbiology and clinical sciences as they relate to the cardiovascular, respiratory, and renal organ systems. The course progresses through five sections beginning with basic concepts necessary for understanding the interrelationships of all three systems, followed by detailed study of medical issues in the three systems individually, and together in the concluding clinical overview session at the end.
Osteopathic Doctoring 2 (4.5 units)
Osteopathic Doctoring provides the basic cognitive and kinesthetic skills for future physicians to provide medical attention in a competent and professionally compassionate fashion. Each Osteopathic Doctoring course builds on the skills and knowledge that was learned in the prior course, incorporating and reinforcing material that is learned in the Integrated Systems & Osteopathic Principles and Practices courses.
Osteopathic Principles and Practices 2 (3.5 units)
The Osteopathic Principles and Practices courses are each a sequential part of a four-semester cumulative body of basic knowledge and skills that spans the first two years of your Osteopathic medical school curriculum. Each course is designed to build on the preceding course and reinforce the basic tenets, philosophy, principles, and practice of osteopathic medicine.
Preclinical Courses: Second Year
Integrated Systems: Neurology/Musculoskeletal (12.5 units)
The Integrated Systems: Neurology/Musculoskeletal course consists of two sections: starting with the neurology section and continuing with the musculoskeletal section.
The neurology system section is composed of 3 major areas: Neuroanatomy, Neurobiology or functional pathways, and Clinical Neurology. The course starts with a focused neuroanatomy section. A solid understanding of the functional anatomy and physiology of the normal central nervous system is essential to the recognition of the pathological processes, lesion localization, diagnosis and treatment of neurological diseases. An integrated functional neurobiology and clinical neurology section follows. It is designed to combine basic information concerning the structure and function of the nervous system with clinical information relevant to the practice of medicine.
The musculoskeletal section provides the knowledge base for understanding the fundamental relation- ship between structure and function in this important system, which is indispensable for a deep comprehension of muscle, bone and joint disorders. This section is focused on the most important musculoskeletal pathologies and their epidemiology, pathophysiology, clinical presentation, diagnostic features and principles of management.
Osteopathic Doctoring 3 (5.5 units)
Osteopathic Doctoring is an integrated and comprehensive course that spans the first two years of the osteopathic medical school curriculum. Each Osteopathic Doctoring course builds on the skills and knowledge that was learned in the prior course, incorporating and reinforcing material that is learned in the Integrated Systems & Osteopathic Principles and Practices courses.
Osteopathic Principles and Practices 3 (2.5 units)
The Osteopathic Principles and Practices courses are each a sequential part of a four-semester cumulative body of basic knowledge and skills that spans the first two years of your Osteopathic medical school curriculum. Each course is designed to build on the preceding course and reinforce the basic tenets, philosophy, principles, and practice of osteopathic medicine.
Integrated Systems: Gastrointestinal, Endocrinology, Reproduction, and Dermatology
(GERD) (13 units)
The Integrated Systems-Gastrointestinal, Endocrinology, Reproductive and Dermatology course develops a deep understanding of biological, diagnostic and therapeutic principles concerning the organs and tissues that make up the gastrointestinal, endocrine, reproductive and dermatologic systems. Specifically, this course will provide students with a strong understanding of basic and clinical sciences as they relate to these organ systems. In addition, this knowledge base will be developed in order to optimize success on board examinations and clinical rotations.
Osteopathic Principles and Practices 4 (2.5 units)
The Osteopathic Principles and Practices courses are each a sequential part of a four-semester cumulative body of basic knowledge and skills that spans the first two years of your Osteopathic medical school curriculum. Each course is designed to build on the preceding course and reinforce the basic tenets, philosophy, principles, and practice of osteopathic medicine.
Osteopathic Doctoring 4 (2.5 units)
As described above Osteopathic Doctoring is an integrated and comprehensive course that spans the first two years of osteopathic medical and school curriculum. Each Osteopathic Doctoring course builds on the skills and knowledge that was learned in the prior course, incorporating and reinforcing material that is learned in the Integrated Systems & Osteopathic Principles and Practices courses.
Preclinical Electives
Global Wellness (Fall & Spring) IPEC 692
This elective brings together the disciplines of psychology, philosophy, integrative medicine (Ayurveda, Traditional Chinese Medicine, Functional Medicine, and Lifestyle Medicine), and behavioral change science to teach the simple, yet effective tools of wellness and personal resiliency for busy people. Activities involve watching videos, building healthy habits, and engaging in group and peer coach check-ins to reflect on your personal progress. Note: Open to all students on campus.
Helping Babies Breathe: Newborn Stabilization in the Developing World (Spring)
OPCC 660
HBB is an evidence-based educational program to teach neonatal resuscitation techniques in resource-limited areas. This course will provide learners with the ability to teach the HBB program during the Global Health summer internship to local individuals who will be providing these services. This course is available to all students enrolled in Global Health Elective, and mandatory for students participating in the Global Health Summer Internship at the Africa sites. Note: Open to medical students only.
Interprofessional Elective in Street Medicine (Spring) IPEC 653
This elective course provides an opportunity for TUC students to develop an understanding of the healthcare needs of the unhoused population, with a specific emphasis on the unhoused population in Vallejo, Ca. This elective will cover enhancing empathetic encounters with patients, presented with an osteopathic lens of addressing the mind-body-spirit connection within each individual, as well as specific topics including substance abuse, chronic illness, wound care, and health insurance. A final reflection assignment will be completed after all other course requirements have been fulfilled (case discussions, volunteering), prior to the end of the semester. In total, this 15 hour elective course involves pre-recorded sessions, interprofessional group work and hands-on experience working with the unhoused community in Vallejo to put into practice the skills acquired. Note: Open only to all students.
LGBTQIA+ Considerations in Healthcare (Fall & Spring) IPEC 650
This is an introductory course for future medical professionals who seek to learn how to become allies to the LGBTQIA+ community as well as other marginalized and underrepresented groups. Students explore the values they bring into the profession and how these values influence and shape their professional lives, including responses to diverse patient cultures. The course uses a multidisciplinary approach to explore the LGBTQIA+ patient and provider experience including clinically relevant topics. Topics include issues relating to trauma informed care, pediatric patient care, LGBTQIA+ Aging, Transgender affirming healthcare, reproductive health and fertility primary care in the LGBTQIA+ community, clinical scenarios LGBTQIA+-related issues from an intersectional perspective. This elective includes Implicit Bias Training and SafeZone training to equip students with communication tools to provide appropriate care with communities that differ from their own.
Life-Saving Hospital Procedures for the Medical Student (Fall &Spring) OPCC 668
This course will involve six sessions, each beginning with a preliminary, interactive PowerPoint presentation followed by a 2-3 hour cadaveric lab demonstration and subsequent medical student performance of 8 such basic, life-saving procedures. Proposed procedures include but may not be limited to Chest Tube Insertion, Cricothyroidotomy, Emergent Open Tracheostomy, Needle Decompression of Chest, Thoracentesis, Pericardiocentesis, Insertion of Central Venous Catheter, Suture Ligation of Bleeding Vessel. Note: Open to only OMS II.
Medical Spanish (Spring) OPCC 650
This beginner's course is offered in the Fall semester with the objective of developing a foundational level of medical Spanish adequate for the student to determine the chief complaint of the Spanish-speaking patient, provide basic medical instructions, obtain information about the patient, and answer the patient's most common questions. These objectives will be achieved through the teaching of Spanish medical terminology, colloquial words and phrases, and some basic grammar, as well as through practice sessions in conducting histories and physicals in Spanish. Note: Open to OMS II students only; before registering for this elective course, please always seek approval from Dr. Menini using the elective course registration form.
OMT Lab (Summer) OMMC 653
This course is a one-semester, a summer course in which students work as OMT demonstration providers in the H-89 OMT lab. Elective participants will work with lab volunteers and a faculty preceptor as they obtain a history, physical exam, and provide an OMT demonstration. Note: Open only to medical students.
Pathways to Success (Fall & Spring) IPEC 690
In Pathways to Success IPEC 690, students will be given the opportunity to learn about and practice evidence-based study strategies, test-taking strategies, mindfulness and time management skills. The course will also cover maintaining well-being, and coping strategies to manage stressful life experiences. This interactive, engaging and self-reflective course meets 6 times during the semester. Students are asked to complete 2 self-care reflections and 2 surveys. This is a pass/no pass course. Note: Open to all students.
Pediatric Obesity Prevention Program (Fall & Spring)
Part A: OPCC 671A - Part B: OPCC 671B
Community Health: Pediatric Obesity Prevention Program [aka, The Project HAPPY (Healthy Attitudes Produce Positive Youth)] elective is an opportunity for Touro students to engage with the community by using patient education and behavioral modification to establish healthy habits and decrease the rate of pediatric obesity. This two-part series provides students with the opportunity to counsel families, employ practice-based learning, and participate in an ongoing research project.
Project HAPPY Elective Part A trains students to lead the family-based behavioral modification research program that is currently underway in Vallejo, CA. Project HAPPY pairs participating Vallejo families with a Touro student health navigator who delivers a predetermined curriculum that addresses attitudes toward health and wellness. Upon completion of Part A, students will be eligible to enroll in Project HAPPY Elective Part B, in which they will partner with a family to guide them through the Project HAPPY curriculum. Note: Completion of Project HAPPY Elective Part A is required for enrollment in Project HAPPY Part B.
Summer Clinical Preceptorship (Summer) OPCC 658
This class is intended to provide students with the opportunity to apply basic science knowledge in a clinical setting during an otherwise non-academic time; i.e., between the first and second years. Students will, with approval of the course coordinator, work with a faculty member of TUCOM, a clinician at another institution, or a licensed physician in the community, in order to observe medical practice in an area of medicine and a clinical setting of their choice.
Taboo: A Study of Medical Bias (Spring) OPCC 665
This course provides an introduction to health care inequalities related to implicit bias and explores 6 common biases in healthcare: gender, obesity, race, sexuality, socioeconomic status, and drug misuse. Topics will be explored through peer-teaching, articles, video clips, reflective writing, and class discussions. Note: Open to all students.
The Healer’s Art (Fall & Spring) OPCC 659
The Healer’s Art, developed by Dr. Rachel Naomi Remen, was first presented at the University of California San Francisco School of Medicine in 1993 and, as of 2008, had been successfully replicated in 59 medical schools in the US and abroad. It addresses the hidden crisis in medicine, the growing loss of meaning and commitment experienced by physicians nationwide under the stresses of today’s health care system. The course is comprised of five interactive sessions entitled: Discovering and Nurturing Your Wholeness; Sharing Grief and Honoring Loss (2); Beyond Analysis: Allowing Awe in Medicine, and The Care of the Soul: Service as a Way of Life. Note: Open to medical students only.
Wilderness Medicine: Mountain Medicine (Fall/Spring) BSCC 672
Requested by Students Only
This course is designed to provide an introduction to the management of common medical issues specific to mountainous environments. The course is comprised of four self-study sections including 1) high altitude illness 2) thermoregulation 3) trauma and improvised medicine and 4) backcountry OMT. There will also be two, one-day interactive sessions in which students will go into the field and practice skills such as improvised litters, splinting, and OMT considerations in the backcountry Note: Requested by students only; open only to medical students.
Science-based Reproductive Health Care IPEC 654
This course is a 1-unit course that meets for 1.5 hour a week for 10 weeks. A maximum of 25 students may enroll. If there is sufficient interest a slightly larger class may be considered. This course is offered to pre-clinical or didactic-year students in any TUC program but is geared to students in the DO, PharmD Program, PA programs. This discussion-based course will cover the physiology, pharmacology, demographics, social policy, and clinical aspects of reproductive health care with special focus on abortion, infertility, and transgender care. The purpose of IPEC 654 is to provide students with an in-depth knowledge base of abortion, infertility, and transgender care that expands upon coverage provided in their core curricula, and allows students to approach these topics knowledgably and confidently in future practice. The cross- disciplinary aspect of this course provides opportunity for interprofessional education and discussion. Through readings and discussion, we will analyze the science-based aspects and terminology of reproductive and gender-affirming care.
Clinical Education
Your third and fourth years will consist of clinical rotations, as well as opportunities for research or further elective study. Third-year clinical rotations include:
- Family Medicine
- Internal Medicine
- Surgery
- Obstetrics and Gynecology
- Pediatrics
- Psychiatry
Fourth-year rotations include:
- Primary Care
- Critical Care
- Emergency Medicine
- Pediatrics
- OB-GYN
- OMM
You'll also have plenty of elective time during your fourth year to complete sub-internships or audition rotations in the specialty of your choice. Many of our students also explore related fields — for example, a family medicine specialist may do a radiology or dermatology rotation.
Specialize Your D.O. Degree
While much of the DO degree path is required coursework, you can expand upon your degree, with a focus on specific areas. You’ll have the opportunity to pay attention to public health (DO/MPH dual degree) and global health (certificate) within your four years at TUC COM, as well as extending your medical school education (an additional year) with a primary care fellowship or OMM fellowship. We also offer a post-graduate fellowship in diabetes.

DO/MPH
Our Doctor of Osteopathic Medicine/Master of Public Health graduates leave TUC with the ability to affect lives on a national and global scale.
Learn More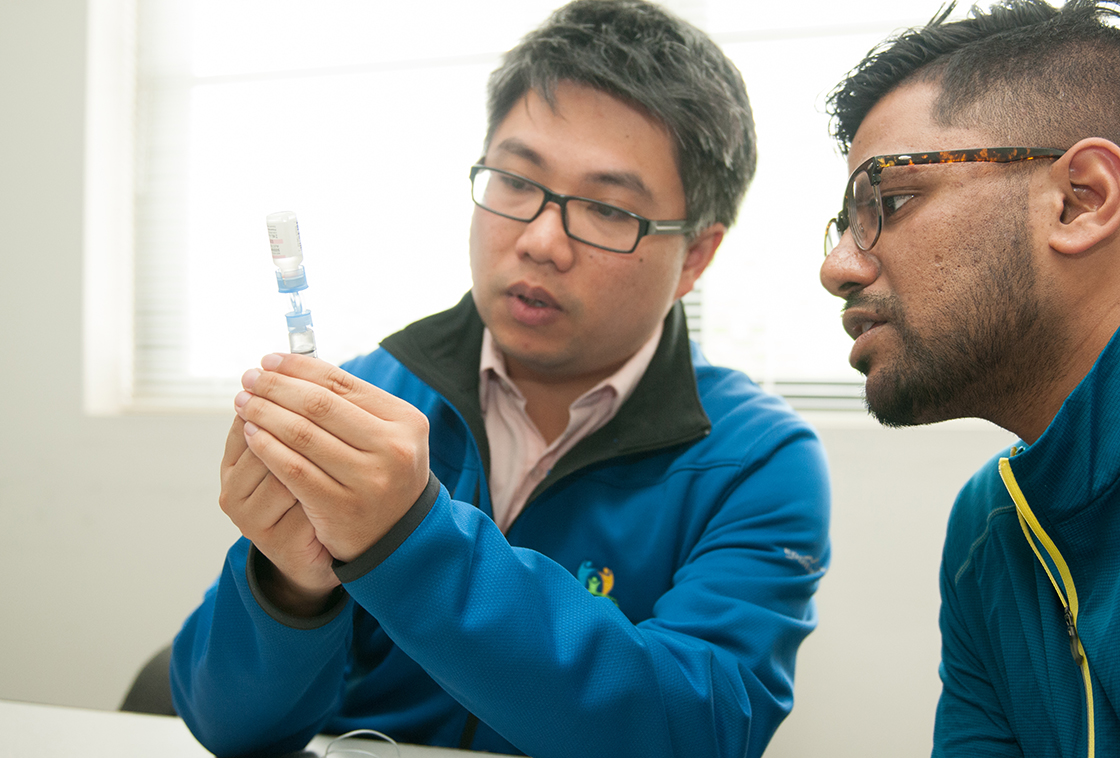
Diabetes Certificate
Learn from a dedicated team of specialists to learn the research and treatment developments for this disease affecting millions of Americans.
Learn More
Global Health Certificate
Our Global Health Pathway students make meaningful changes around the world at locations in Africa, India, Mexico, Taiwan, and Israel.
Learn More
OMM Fellowship
Fellows participate in additional clinical, didactic, and research experiences, and develop and deliver OMM medical education to peers.
Learn More
Primary Care Fellowship
The Primary Care Teaching Fellowship will refine your skills as a future physician and medical educator. This is an ideal opportunity for anyone interested in teaching and academic medicine.
Learn More